The best EHR for Family Practice
A.I. Driven efficiency and time saving for your family practice Praxis offers the best EHR…
Praxis is proud to be in the Capterra Top 20 EMR report
Praxis EMR earned the #1 score in Review Ratings with a perfect 5 Star rating!…
Software Advice Ranks Praxis #1 in EHR Usability
Woodland Hills, Calif., February 5th, 2019 Praxis EMR, a leading provider of Electronic Health Records (EMR/EHR)…
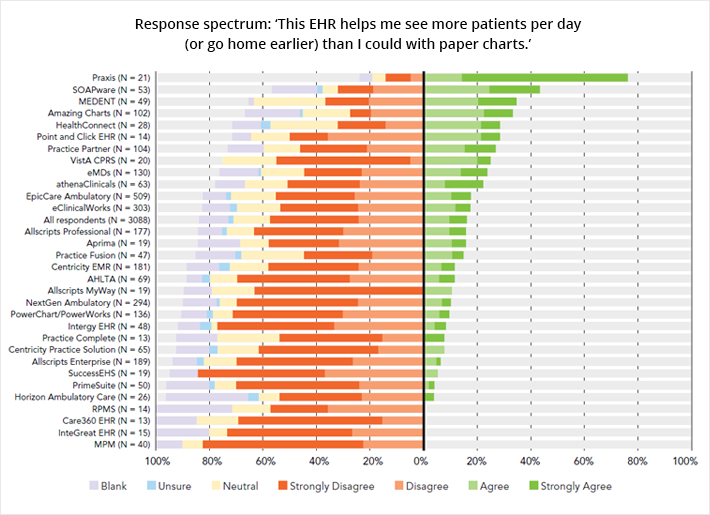
American College of Physicians (ACP) EHR User Satisfaction Survey Ranks Praxis EMR #1
The ACP’s AmericanEHR Partners ranks Praxis EMR the No. 1 EHR in User Satisfaction and…
Software Advice Ranks Praxis #1 in EHR Usability
Encino, Calif., August 24th, 2018 –Software Advice by Gartner, the world’s leading research and advisory company…
Considering Concierge Medicine? Praxis can help your practice
A recent study by the American Medical Association (AMA) found that physicians spend twice as…
Software Advice Ranks Praxis as one of the Top 3 EMR Solutions
Keeping on top of the electronic medical records (EMR) software market can be intimidating for…
Best EHR Systems for Small Practices
When selecting an electronic healthcare record (EHR) system for your small practice, you might think…
Do you have EHR Burnout?
A recent study by the American Medical Association (AMA) shows that physicians spend twice as…
Physician EHR Dissatisfaction Linked to Template Technology
With the majority of US doctors now having used an Electronic Medical Record (EMR/EHR), physician…
EMR versus EHR
What a difference a single letter makes Over the past few years medicine has witnessed…
Praxis EMR is the Number One Rated EHR in Major User Satisfaction Surveys for 2015
AAFP Physicians Give Praxis EMR Highest Rating when Switching EHRs; Black Book Ranks Praxis Number…