The Hidden Dangers of Conventional Ambient AI in Medicine
Why Smart Physicians Choose Praxis Instead In today’s high-tech healthcare world, Conventional Ambient AI—also known…
Beyond Charts & Clicks: Unleashing the Power of EMR for Patient Engagement
If you work in healthcare, you have probably heard of EMR systems and how helpful…
7 Top-Rated EMR Software
From stacks of patient files and manual screenings to creating and sharing electronic documents, using electronic…
Health 3.0 and your EHR
Dr. Zubin Damania on Physician “Burnout” Dear Colleague, Doctor Damania is exactly right. Praxis is…
Physicians choose their Top 10 EHR systems for 2021
Looking for the best Electronic Medical Record (EMR/EHR) for your practice? Compare the top 10…
Software Advice Ranks Praxis EMR #1 in Usability and Customer Recommended
Software Advice by Gartner, the world’s leading research and advisory company featuring online reviews of…
The Best EHR’s of 2021
Compare the top 10 EHR vendors in different care settings. Comparison includes Epic, AllScripts, NextGen,…
American College of Physicians (ACP) EHR User Satisfaction Survey Ranks Praxis EMR #1
The ACP’s AmericanEHR Partners ranks Praxis EMR the No. 1 EHR in User Satisfaction and…
The Benefits of Praxis Electronic Medical Records
https://www.reddit.com/r/HealthcareMedicalIT/comments/y7tkcq/the_benefits_of_praxis_electronic_medical_records/
Software Advice Ranks Praxis #1 in EHR Usability and Customer Satisfaction
Software Advice by Gartner, the world’s leading research and advisory company featuring online reviews of…
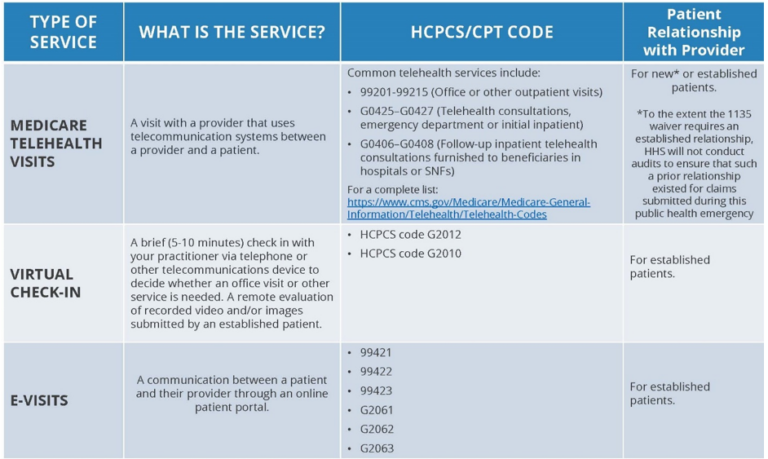
Medicare Telemedicine Health Care Provider Fact Sheet
Medicare coverage and payment of virtual services INTRODUCTION: Under President Trump’s leadership, the Centers for…
The best EHR for Primary Care
A.I. Driven efficiency and time saving for your Primary Care practice Praxis offers the best…